When you can’t detect odors, it’s usually temporary. But not always…
Can you imagine not being able to smell a hot cup of coffee, the post-rain scent of a fall morning, or just-cut grass on a sunny, summer afternoon?
You might not miss the stinky, wet smell of your dog after a romp in the mud – but then again, losing your sense of smell for any amount of time can be disorienting and emotionally troubling.
Often, a temporary lack of sensory perception is caused by a cold or sinus infection. Once you recover, your sense of smell generally returns full-on. But what if it doesn’t come back?
If your olfactory senses seem distorted—was it caused by COVID-19? Or is it related to some other disease? We talked with Dr. Ryan Wood of NW Regen in Portland to find out more about the types of olfactory conditions he encounters with patients at his regenerative health clinic.

Several causes can change or distort the sense of smell.
What Causes a Lost or Distorted Sense of Smell?
People’s sense of smell can change or be distorted. Several conditions are:
- Anosmia: The complete inability to smell.
- Hyposmia: A reduced ability to smell.
- Parosmia: A change in how you perceive smells, such as when something familiar smells distorted or something that normally smells pleasant now smells bad.
- Phantosmia: The sensation of smelling something that isn’t there.
There are also several diseases that can affect your sense of smell, including:
- Upper respiratory infection: A common cause of neural olfactory loss, especially in women and people 65+.
- Sinusitis: A physical blockage in the nose that prevents odors from reaching the olfactory epithelium.
- Alzheimer’s disease: Smell changes are more common in the middle and severe stages of the disease.
- Parkinson’s disease: Up to 95% of people with Parkinson’s report varying degrees of smell loss.
Other diseases and conditions that can affect your sense of smell include kidney failure, serious liver disease, obesity, diabetes, hypertension, and malnutrition. Also, Anosmia and Parosmia have been seen to be caused by Long COVID.
Long COVID Symptoms: Anosmia and Parosmia
Long COVID is a post-viral syndrome that continues to baffle the medical community as a complex and evolving health issue. Among myriad long-term COVID symptoms, anosmia and parosmia stand out as the most common. Understanding these conditions is crucial. For those experiencing them and also for healthcare professionals and the general public.
These conditions relate to the loss of smell (anosmia) and distortion of smell (parosmia). Both conditions can significantly impact your quality of life and can affect mental health, nutrition, and even safety. At NW Regen, Dr. Ryan Wood treats anosmia and parosmia with regenerative health therapies that are having significant impact on his patients.
In this article, we aim to shed light on anosmia and parosmia as symptoms of Long COVID, delve into their prevalence, their potential treatments, and some coping strategies. Join us as we explore the world of Long COVID, possible treatments, and how they impact the senses.
Understanding Long COVID’s Impact on the Senses
Long COVID (also known as “post-acute sequelae of SARS-CoV-2 infection”) encompasses a range of symptoms that persist long after the acute phase of COVID-19 has ended.
Olfactory dysfunction is notably common. Many individuals report a prolonged loss or alteration of their senses, known as anosmia and parosmia, respectively. “One thing I often hear is that people complain of putrid, chemical, and smoke-like smells,” says Dr. Wood. “Peanut butter and meat often are described as rancid, and occasionally the only taste long COVID sufferers have are for sweet or sugary foods.”
Loss of smell and taste are more than just minor inconveniences, as they can:
- Significantly alter daily experiences.
- Affect an individual’s emotional wellbeing.
- Lead to nutritional challenges.
- Raise safety concerns (e.g. being unable to detect smoke or gas leaks).
“To say it was life changing is almost an understatement.”
I can’t say enough good things about Dr Wood. I had been suffering from severe anxiety and Panic attacks brought on by Long COVID. Dr Wood really takes the time to understand his patients. He is a great listener and very well informed on treatment protocols.
NW Regen patient, Karl A.
Anosmia and Parosmia Explained
Both conditions can severely impact quality of life and mental health.
- Anosmia: No sense of smell at all.
- Parosmia: Smells become distorted and unfamiliar.
Anosmia refers to the complete loss of smell. It often results in a diminished sense of taste as well. This condition can be disorienting and distressing for those affected.
“When you can’t detect odors, it’s usually temporary from a cold or sinus infection,” explains Dr. Wood. “Yet sometimes, it may be from a condition that interferes with signals sent from scent cells to your brain, or from serious medical issues like diabetes or traumatic brain injury.”
Parosmia, on the other hand, involves the distortion of smell. Familiar scents turn unpleasant or unrecognizable. These alterations can linger for months or even longer.
“A distorted sense of smell occurs when smell receptor cells in your nose don’t detect odors or transmit them to your brain,” explains Dr. Wood. “Causes include bacterial or viral infections, head trauma, neurological conditions, and COVID-19. Parosmia is usually temporary but can be permanent.”

With parosmia, familiar scents turn unpleasant or unrecognizable.
Olfactory Dysfunction in Long COVID Patients
Studies show that anosmia and parosmia affect a significant portion of long COVID sufferers.
“Olfactory dysfunction is a common symptom among those with long-term COVID-19,” says Dr. Wood. “Many patients experience changes in their sense of smell and taste. The prevalence is higher than in typical post-viral syndromes.”
These sensory disruptions can persist even after other COVID-19 symptoms disappear. This highlights the need for recognition and targeted interventions for affected individuals.
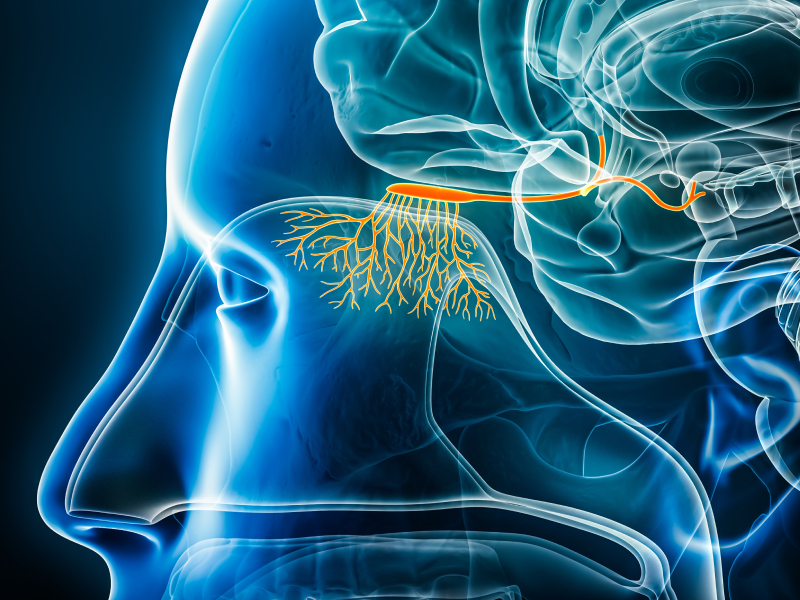
An inflamed olfactory bulb may impact smell and taste.
How COVID-19 Affects Biological Mechanisms
COVID-19 impacts the olfactory system through direct and indirect means. The virus can attack the cells in the nasal cavity. This leads to a loss of smell and subsequent taste disruptions.
Scientists suggest that COVID-19 might cause neurological impacts, affecting smell and taste pathways. This contributes to the prolonged loss of these senses in long-term cases.
Research is ongoing to fully understand these mechanisms. A deeper understanding could aid in developing effective therapies for olfactory dysfunction.
“The olfactory bulb, a crucial structure in scent processing, may experience inflammation due to the virus,” explains Dr. Wood. “This inflammation disrupts normal smell transmission to the brain.”
At NW Regen, we treat the root cause with a tailored regimen of therapies and rehabilitation, including the Stellate Ganglion Block, which has been shown to help with the distress associated with loss of smell in addition to helping to restore the sense over time.”
Dr. Ryan Wood is the most experienced specialist in Stellate Ganglion Blocks on the west coast, with 2000+ procedures performed since specializing in SGB injections starting in 2017.
Psychological & Social Tolls of Anosmia & Parosmia
Loss of smell and taste significantly affects mental health. Many individuals feel isolated and distressed due to these changes.

A lack of enjoyment in meals can impact social interactions.
“Food is a big part of our social life as humans,” says Dr. Wood. “Social gatherings often center around food and scents. This can make individuals with anosmia and parosmia feel excluded. It’s crucial for loved ones and communities to offer understanding and support.”
The persistent sensory loss from anosmia and parosmia can:
- Alter daily routines and life satisfaction.
- Create stress for those affected.
Lead to anxiety and depression.
Treatment of Long COVID Olfactory Disorders
Managing anosmia and parosmia involves a multi-faceted approach. Medical professionals recommend several treatments to aid recovery. These aim to help individuals regain their senses over time.
It’s essential for patients to work closely with healthcare providers. A tailored approach can provide the best chance of improvement.
- Corticosteroids are often prescribed to reduce inflammation. This may improve olfactory function in some patients. However, their effectiveness varies between individuals.
- Olfactory training has gained popularity as a rehabilitation method. It involves repeatedly smelling specific scents to stimulate the olfactory system. Consistency and patience are key for success with this technique.
Other potential treatments include vitamin supplements and the use of smell retraining kits.
SGB Therapy for Long COVID Olfactory Disorders
Alternative therapies that are having success with long haulers include an injection therapy known as the Stellate Ganglion Block, which is available at NW Regen from the west coast’s leading expert, Dr. Ryan Wood.
“Patients tell us: ‘It’s been great to get affirmation that I’m not the only person with these issues’, ‘I kept being told it was all in my head’ or ‘There’s comfort in knowing I’m not alone,’ says Dr. Wood. “Don’t suffer in silence. Relief may be available in less than 30 minutes with the Stellate Ganglion Block therapy. Come visit to see what’s causing your condition and if you are a candidate for this therapy that addresses your discomfort and promotes natural healing.”
At NW Regen, tailored treatment plans address many symptoms faced by long haulers, promoting natural healing that restores health and vitality while combating the fatigue and depression many patients experience caused by Long COVID.
The Role of Olfactory Training and Rehabilitation
Olfactory training is crucial in managing anosmia and parosmia.
This technique encourages the olfactory system to recover. It’s a practical, non-invasive approach with promising results. The process involves exposure to a variety of scents.

Lemon, rose, clove, and eucalyptus are commonly used.
Over time, repeated exposure can stimulate nerve pathways and potentially restore smell.
Patience is essential during rehabilitation. Participants often notice gradual improvements. Regular practice increases the likelihood of regaining olfactory senses. Consistent training can be key to recovery for many patients affected by long COVID symptoms.
Coping Strategies & Support for Anosmia & Parosmia
Living with anosmia and parosmia can be challenging. However, various coping strategies can ease the burden. Adapting daily routines can significantly improve quality of life.

Finding support is crucial for individuals dealing with these sensory losses.
Support groups and online communities offer valuable resources and a sense of belonging. Sharing experiences with others in similar situations can provide comfort and guidance.
Here are some effective coping strategies:
- Olfactory training: Engage in smell exercises to potentially recover some function.
- Safety measures: Use smoke detectors and food freshness labels more frequently.
- Mental health care: Seek professional support for emotional challenges.
Individuals should explore these strategies to foster improved well-being and resilience.
The Road Ahead for Sensory Loss from Long COVID
The journey of understanding and managing long COVID symptoms continues to evolve. Anosmia and parosmia remain significant challenges.
Healthcare providers and researchers must collaborate on solutions. Patient-reported outcomes will play a vital role in guiding these efforts. With continued support and awareness, those affected can find hope and recovery. The road may be long, but advancements in care and understanding offer a promising future for people dealing with sensory loss.
To learn more about NW Regen’s treatments for sensory loss, book a consultation today.
NW Regen
We offer regenerative and interventional medicine – tailored to empower you with a more vibrant, active lifestyle.


